Understanding What Is Insulin Resistance: Causes, Symptoms, and Treatments

Insulin resistance occurs when your muscle, fat, and liver cells don’t respond properly to insulin, resulting in higher blood sugar levels. This can lead to prediabetes and Type 2 diabetes. In this guide, we’ll cover “what is insulin resistance”, its causes, symptoms, how it’s diagnosed, and treatment options available, so you can improve your metabolic health and well-being.
Key Takeaways
-
Insulin resistance is when cells in muscles, fat, and liver don’t respond to insulin properly, causing higher blood glucose levels and possibly leading to prediabetes and Type 2 diabetes.
-
Major causes of insulin resistance include excess body fat, particularly around the abdomen, physical inactivity, and genetic factors, necessitating a focus on lifestyle changes and genetic awareness for prevention.
-
Management and reduction strategies for insulin resistance involve adopting a healthy diet low in refined carbohydrates and sugars, engaging in regular physical activity, and considering medications and natural supplements as appropriate.
Understanding Insulin Resistance
Insulin resistance occurs when cells in muscles, fat, and liver don’t respond as they should to insulin, leading to higher blood glucose levels and increased insulin production. Insulin is a hormone made by the pancreas that helps glucose enter cells for energy. When cells become insulin resistant, the pancreas has to produce more insulin to manage blood glucose levels, a condition known as hyperinsulinemia. This excess insulin production can worsen insulin resistance over time.
If insulin resistance is severe and the pancreas can’t produce enough insulin, it leads to elevated blood glucose levels, which can cause prediabetes and Type 2 diabetes. The condition can be temporary or chronic and is treatable in some cases. Grasping the development process of insulin resistance and its consequences is essential for its effective diagnosis and management.
How Insulin Works in the Body
Insulin plays a vital role in regulating blood sugar levels by facilitating glucose uptake into cells. After a meal, insulin stimulates glucose storage in the liver as glycogen and enhances the facilitated diffusion of glucose into most tissue cells. This process helps decrease blood glucose levels by allowing cells to absorb blood glucose for energy or storage.
In the liver, insulin stimulates glycogenesis, the process of converting glucose to glycogen. Additionally, insulin promotes the conversion of glucose to ATP, providing energy for cellular functions. Comprehending insulin’s function aids in recognizing the effect of insulin resistance on glucose metabolism and general health.
Causes of Insulin Resistance
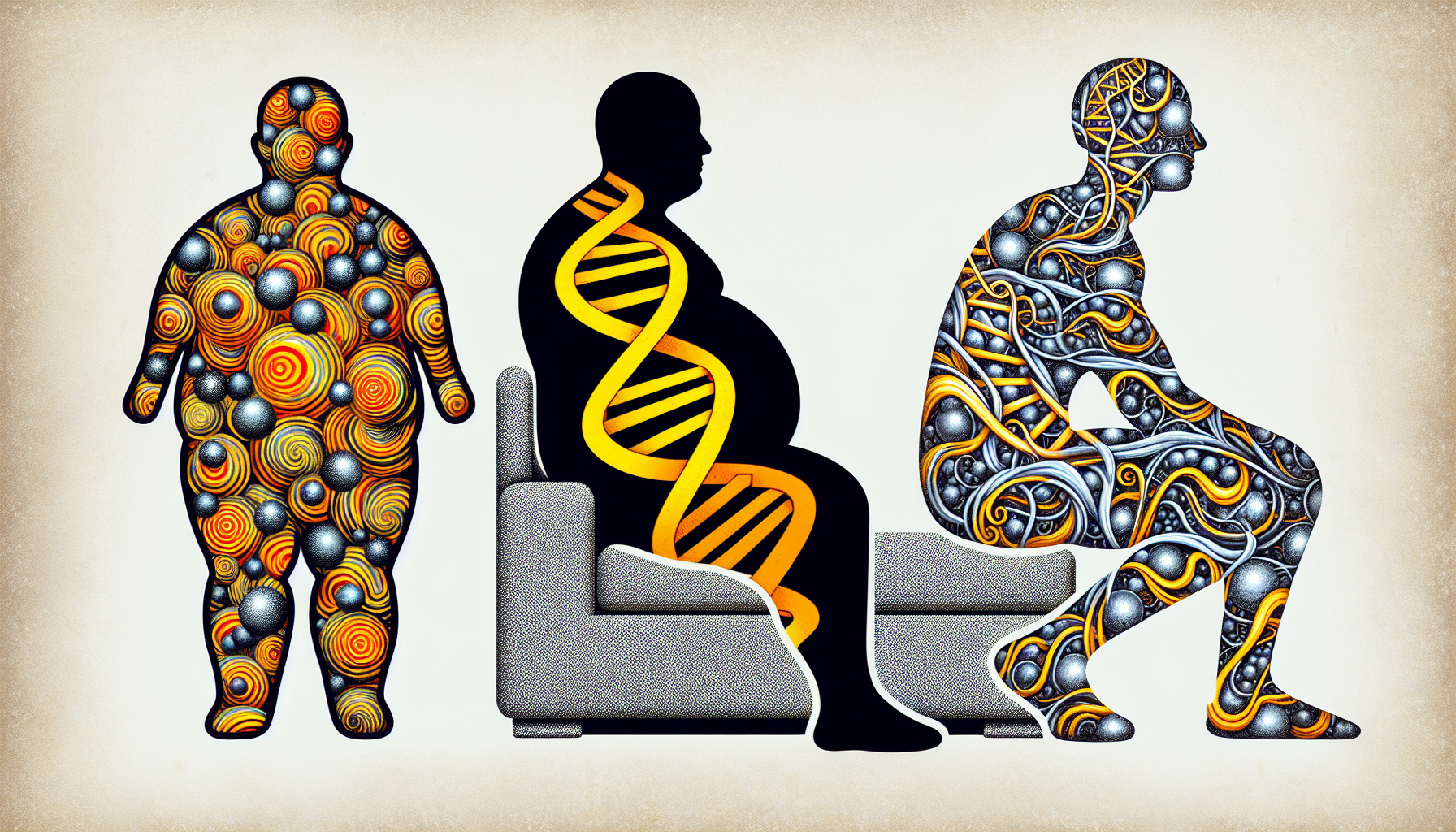
Insulin resistance is primarily caused by excess body fat, processed foods, seed oils and physical inactivity. The accumulation of fat, especially around the abdomen, significantly contributes to insulin resistance. Visceral fat releases substances that reach the liver through the portal vein, contributing to insulin resistance. Additionally, a lack of physical activity is a major contributor to developing insulin resistance. Over the past few decades, the food pyramid that was introduced as dietary guidelines containing the intake of 60% of your calories from carbohydrates, has dramatically spiked obesity and insulin resistance rates, leading to type II diabetes and heart disease epidemic all across the globe. If you prefer to learn more about this topic, check this video by Dr Elena Seranova.
Genetic factors also play a crucial role. Specific genetic markers and family history can influence an individual’s susceptibility to insulin resistance. Being aware of these causes aids in formulating effective strategies to fight insulin resistance.
Excess Weight and Fat Tissue
Visceral fat is particularly harmful because it:
-
Infiltrates spaces around organs, causing insulin resistance through inflammatory processes
-
Produces hormones and other substances that contribute to chronic inflammation
-
Is implicated in insulin resistance
-
Can impair insulin sensitivity and exacerbate the condition
Losing excess body weight, especially around the abdomen, helps in combating insulin resistance. By reducing visceral fat, the inflammatory processes and hormone imbalances associated with insulin resistance can be mitigated, improving overall health.
Physical Inactivity
Living a sedentary lifestyle can greatly increase the risk of developing insulin resistance. This is the reason why integrating regular physical activity into our daily routines is necessary. Lack of physical activity contributes to impaired insulin sensitivity, making it harder for the body to absorb glucose. This can lead to higher blood sugar levels and increased insulin production.
Engaging in regular physical activity can help reduce insulin resistance by making muscle cells more capable of absorbing glucose. Exercise also assists in weight management, which is vital for both prevention and reversal of insulin resistance.
Genetic Factors
Genetic predisposition plays an essential role in determining an individual’s susceptibility to insulin resistance. Specific genetic markers, such as mutations in the insulin receptor gene, have been identified as contributing factors. Hereditary conditions like polycystic ovary syndrome (PCOS) are also associated with increased risk.
A family history of diabetes or insulin resistance can significantly increase an individual’s likelihood of developing the condition. Comprehending these genetic factors can assist in early detection and management of insulin resistance.
Symptoms of Insulin Resistance
Insulin resistance and prediabetes typically do not display any symptoms. It is important to consult a healthcare professional for proper evaluation and management. This makes it challenging to diagnose without proper medical tests. Some individuals with prediabetes may observe darkened skin in certain areas, such as the armpits and the back and sides of the neck. This condition is known as acanthosis nigricans.
In addition, skin tags often appear in these areas as well. They are small skin growths. While these symptoms are not definitive indicators, they can be warning signs that prompt further medical evaluation. As a rule of thumb, the vast majority of people that have already developed insulin resistance will have excess fat around their waist though. So if you can already see some love handles around your waist, this is your sign to evaluate what are you doing for your health on a daily basis, and how can you refine your decision making process when it comes to food and lifestyle choices. So the most efficient way to manage insulin resistance is to lose weight. Although the optimal approach will always be an individualised one, the easiest way to do this is probably by reducing the intake of processed foods, carbohydrates and seed oils while exploring an intermittent fasting regime that suits you best.
Diagnosing Insulin Resistance
Doctors use various blood tests to diagnose insulin resistance and prediabetes. Common tests include fasting blood glucose, A1C, and oral glucose tolerance tests. These tests help in identifying high blood sugar levels and assessing how well the body manages glucose.
Early detection of insulin resistance is crucial as it allows for timely intervention to prevent the progression to Type 2 diabetes and other complications. Comprehending the diagnostic process highlights the significance of regular health check-ups.
Fasting Plasma Glucose Test
The fasting plasma glucose test requires the individual to fast for at least 8 hours before the blood sample is taken. A normal fasting plasma glucose level for individuals without diabetes ranges from 70 to 99 mg/dL. Levels between 100 and 125 mg/dL indicate prediabetes.
A fasting glucose level over 100 milligrams per deciliter (mg/dL) can suggest insulin resistance and may require further testing to confirm the diagnosis.
A1C Test
The A1C test measures average blood sugar over the previous 2-3 months to help diagnose prediabetes or diabetes. This test calculates the average blood glucose over the past three months, providing a more comprehensive view of blood sugar management.
Interpreting these results aids in evaluating long-term blood sugar control and the probability of developing diabetes.
Oral Glucose Tolerance Test
The oral glucose tolerance test is a diagnostic tool used to identify prediabetes or diabetes. It involves measuring blood glucose levels after consuming a glucose solution. This test involves:
-
Measuring blood glucose levels before consuming a sugar-rich drink
-
Consuming the sugar-rich drink
-
Measuring blood glucose levels at regular intervals after consuming the drink to monitor how efficiently the body processes glucose.
A blood sugar level of 140-199 mg/dL after 2 hours indicates prediabetes, while 200 mg/dL or higher indicates diabetes. This test offers significant insights into the body’s sugar intake management.
Risk Factors for Developing Insulin Resistance
Several factors increase the risk of developing insulin resistance. As insulin resistance develops, excess body fat, particularly around the abdomen, significantly contributes to the condition. Lack of physical activity is another primary lifestyle risk factor.
Genetic predisposition, a family history of diabetes, and certain health conditions like metabolic syndrome and polycystic ovary syndrome (PCOS) also increase the risk. Recognizing these risk factors facilitates the adoption of preventive measures at earlier stages. It is worth noting that while type I diabetes has indeed a strong genetic component, due to the lack of insulin production in the patient's body, we now understand that type II diabetes is now considered as something that can be reversed as multiple cases indicate just by adjusting someone's diet. With many thousands of patients switching to a low carb or no carb diets, and enjoying the benefits of primal, carnivore diets, type II diabetes has been documented to be reversed in many occasions. Unfortunately, not all medical practitioners are looking into this integrative medicine approach, but the awareness of the fact that the patient actually has much more control over their health is now spreading.
Health Implications of Insulin Resistance
Prediabetes occurs when blood glucose levels are higher than normal but not high enough to be classified as diabetes, often preceding Type 2 diabetes. Insulin resistance can often lead to prediabetes. Over time, it may progress to Type 2 diabetes.
Insulin resistance can also lead to metabolic syndrome, nonalcoholic fatty liver disease (NAFLD), and cardiovascular disease. These health implications emphasize the necessity for early detection and management of insulin resistance.
Strategies to Reduce Insulin Resistance

Adopting a healthy diet, engaging in regular physical activity, and considering medication options can help manage and reduce insulin resistance. Weight loss is another effective strategy to combat insulin resistance.
Lifestyle changes around eating, physical activity, and weight management can significantly lower the chances of developing insulin resistance or prediabetes. The implementation of these strategies can assist in reversing insulin resistance and enhancing overall health. Our community of NMN Bio-Hackers already knows how important insulin sensitivity is, and how offseting insulin resistance is crucial for longevity. If you can't manage your weight and your insulin levels, you can forget about longevity.
Healthy Diet
Consuming a balanced diet low in refined carbohydrates and sugars does improve insulin sensitivity. Incorporating foods rich in omega-3 fatty acids, such as fatty fish, can also enhance insulin sensitivity.
Cutting down on sugary beverages and snacks reduces the risk of developing insulin resistance. Eating a diet high in protein and fats, but low in carbohydrates, a physiologically relevant diet for the human species, is proven to balance insulin levels, as there is no excess amount of carbohydrates to spike your insulin in the first place. Makes sense? The Carnivore Diet book by Dr Shawn Baker is an excellent book that acts as a resource if you are interested in the subject and would like to learn more about this simple, yet powerful lifestyle change. Another textbook would be the Deep Nutrition book by Dr Catherine Shanahan that describes the evolution of the human body throughout millennia, depending on the food sources available. An exciting, easy read that is unbiased towards any particular diets, but describes the history of mankind from an interesting angle, and makes you think about your current nutritional choices.
Regular Physical Activity
Engaging in regular physical activity can help prevent and reverse insulin resistance by making cells more responsive to insulin. Strength training exercises help in building muscle mass, which enhances insulin sensitivity.
Physical activity reduces insulin resistance by making muscle cells more capable of absorbing glucose. This effectively aids in blood sugar level management.
Medication Options
Medications like metformin and thiazolidinediones can improve insulin sensitivity and reduce insulin resistance. Metformin is a commonly prescribed medication that helps reduce insulin resistance.
These medications work by making the body’s cells more sensitive to insulin, thereby improving glucose metabolism. They are particularly beneficial for individuals with a history of gestational diabetes, younger adults, and people with obesity.
Natural supplements to combat insulin resistance

Natural supplements like Berberine can help with:
-
Reducing sugar cravings
-
Improving blood glucose regulation
-
Lowering bad cholesterol
-
Improving metabolic rate after a few weeks of supplementation.
The combination of Berberine and Milk Thistle can enhance the body’s reaction to carbohydrates and regulate blood glucose levels. Regular supplementation can activate key longevity pathways, helping cells function better.
Preventing and Reversing Insulin Resistance

Lifestyle changes, such as weight loss, healthy eating, and regular exercise, can lower the risk of developing insulin resistance or prediabetes. Losing 5 to 7 percent of starting weight can significantly help in preventing diabetes.
A balanced diet low in refined carbohydrates and sugars, along with increased fiber intake, can improve insulin sensitivity. Engaging in aerobic exercises and high-intensity interval training (HIIT) effectively manages insulin levels.
Clinical Trials and Research
Clinical trials have a pivotal part in progressing medical treatments and enhancing life quality for individuals with chronic illnesses, including insulin resistance. These trials aim to find more effective prevention and treatment methods. For example, a research trial using Tc-99m-tilmanocept is evaluating kidney changes in diabetics and those with hypertensive kidney disease. Such studies help in understanding the broader implications of insulin resistance and associated diseases.
Several clinical trials are currently open for insulin resistance and prediabetes, focusing on validating screening approaches and testing new medications. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into a wide range of diseases and conditions. This includes insulin resistance. Participating in these trials can provide patients with access to cutting-edge treatments and contribute to medical research advancements.
Summary
Understanding insulin resistance is fundamental to managing and preventing related health issues. It begins with recognizing how insulin functions, identifying the causes and symptoms of insulin resistance, and knowing the diagnostic methods available. Risk factors like excess weight, physical inactivity, and genetic predisposition play a significant role in developing the condition.
Health implications of insulin resistance include prediabetes, Type 2 diabetes, metabolic syndrome, and cardiovascular diseases. However, strategies such as adopting a healthy diet, engaging in regular physical activity, and considering medication options can significantly reduce insulin resistance. Natural supplements like Berberine offer additional support. Emerging literature is pointing towards NMN, an anti-aging supplement also increasing insulin sensitivity in pre-diabetic women. When looking at it from the longevity perspective, combining Berberine, NMN and TMG (another longevity supplement that supports liver function) can be an excellent strategy to maintain your ideal weight, combat insulin resistance and increase your healthspan, aka the amount of years you spend in good health. By optimising your metabolic health with these supplements, you maximise good health for the years to come, so you can attend more birthdays and spend precious moments with your loved ones. Proactive management through lifestyle changes can help reverse insulin resistance and lead to a healthier life.
Frequently Asked Questions
What is insulin resistance?
Insulin resistance happens when cells don't respond properly to insulin, causing increased insulin production and higher blood glucose levels.
How can I tell if I have insulin resistance?
You can tell if you have insulin resistance by checking for symptoms such as darkened skin in the armpit or on the back and sides of the neck, known as acanthosis nigricans. If you notice these changes, it's important to consult with a healthcare professional for further evaluation and management.
What tests are used to diagnose insulin resistance?
To diagnose insulin resistance, common tests like fasting plasma glucose, A1C, and oral glucose tolerance tests are used to measure blood sugar levels and assess how well the body manages glucose.
Can lifestyle changes help reverse insulin resistance?
Yes, lifestyle changes such as adopting a healthy diet, engaging in regular physical activity, and losing weight can help reverse insulin resistance.
Are there any natural supplements that can help with insulin resistance?
Yes, Berberine and Milk Thistle are natural supplements that can help improve insulin resistance and regulate blood glucose.
Researched and reviewed by Dr Elena Seranova, Ph.D.
Dr Seranova holds a master's degree in Translational Neuroscience from the University of Sheffield, UK, and a Ph.D in Stem Cell Biology and Autophagy from the University of Birmingham, UK. She is a published author in multiple peer-reviewed journals, including Cell Reports and Developmental Cell.
LEARN MORE!






Leave a comment